A 31-year-old malnourished male with a history of methamphetamine use was brought to the trauma bay in cardiac arrest following a motor vehicle collision. He underwent an emergent resuscitative thoracotomy with aortic cross-clamping and was transported to the operating room for definitive management.
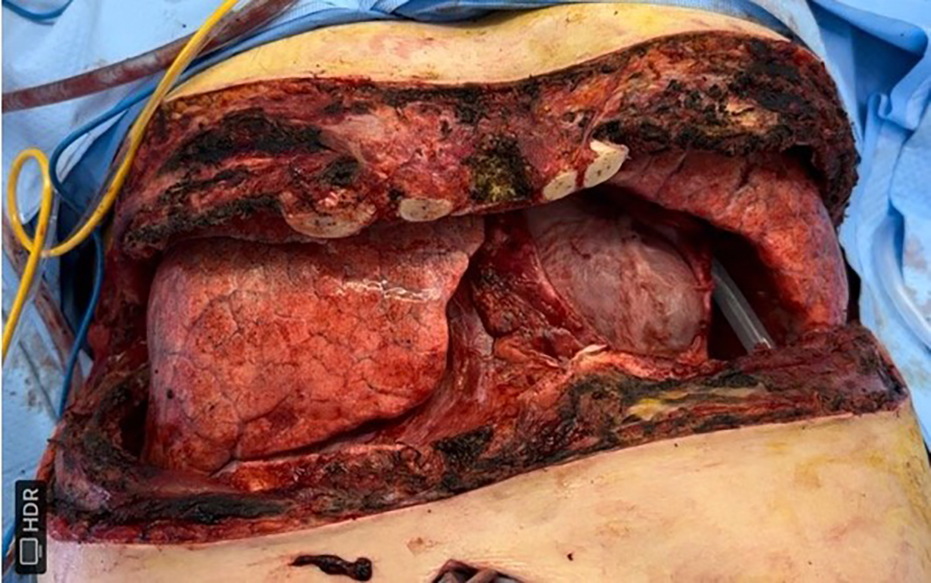
Initial operative findings and interventions: Converted to a clamshell thoracotomy with non-anatomic bilateral lower lung resections for hemorrhage control, exploratory laparotomy with complex hepatorrhaphy and liver packing, and temporary chest and abdominal closure after >5 L blood loss.
Subsequent course: Required multiple re-operations within 36 hours for ongoing hemorrhage control, followed by definitive chest wall reconstruction with open reduction internal fixation (ribs 5–8 and sternum), intercostal nerve cryoablation, and STRAVIX tissue placement.
Complication and re-intervention: One month postoperatively, hardware exposure and wound dehiscence developed. The patient underwent sharp debridement and complex flap closure (39 cm²) with application of GRAFIX and STRAVIX dressings and negative-pressure wound therapy.